Exploring factors influencing coping with uncertainties in medical practice: insights from residents’ experience
Article information
Abstract
Purpose
Despite attempts to teach medical students and trainees about uncertainty in medical practice and how to tolerate it, studies on how to promote tolerance to uncertainty remain scarce. this study aims to investigate factors that could foster residents’ tolerance to uncertainty.
Methods
The authors used data sources, including semi-structured individual in-depth interviews with 20 medical residents working in two tertiary university hospitals. Inductive analysis of interview records determined key themes, identified categories, and performed a theoretical-type analysis of the participants’ coping behaviors according to the attributes of uncertainty tolerance.
Results
Two characteristics of residents which could lead to constructive coping with uncertainty were discovered: (1) communicative/collaborative behavior with their colleagues, superiors, and patients and (2) self-reflective/self-directed attitude in their medical practice. Both were used to classify four types of uncertainty coping behaviors: adaptive, self-contained, submissive, and isolated.
Conclusion
Fostering communicative/collaborative behaviors and self-reflective/self-directed attitude throughout the training period may result in residents being more tolerant of uncertainties in medical practice.
Introduction
Uncertainty pervades all aspects of medicine [1]. The causes of uncertainty in medicine include knowledge limitations, diagnosis challenges, treatments and outcome ambiguity, and the inability to predict patient responses [2]. Fox [3] indicated that medical students’ uncertainties derived from personal ignorance, limitations of available medical knowledge, and difficulties distinguishing beween the two [3]. Beresford [4] suggested that medical uncertainty arises from technical, personal, and conceptual sources. While technical uncertainty arises from the lack of scientific information, personal uncertainty arises from ignorance of patients’ thoughts, feelings and desires. Conceptual uncertainty arises from incompatibility between reality and concepts [4].
Physicians’ tolerance for uncertainty impacts their well-being and patient care quality [2,5,6]. Doctors with a low tolerance for uncertainty result in higher numbers of unnecessary hospital referrals and laboratory tests. They exhibit higher anxiety levels, burnout symptoms, and low satisfaction levels in their medical practice, [7,8] and tend not to share their uncertainties in making treatment decisions [2].
Typically, university hospitals serve as primary locations for acute and critical illness management involving complex medical conditions, inevitably exposing trainees to medical practice uncertainty. As trainees’ uncertainty and tolerance to it can influence professional development and eventually the quality of patient care, it seems crucial to reveal the factors that could affect tolerance to uncertainty.
Despite the abundant research published in recent years about trainees’ experiences [9–16], there is seemingly no study that specifically reveals factors or characteristics of residents that could affect tolerance to uncertainty. Therefore, by analyzing residents’ experiences of uncertainties in practice, this study aims to investigate residents’ characteristics to which constructive coping with uncertainty could be attributed which may in turn result in tolerance to uncertainty.
Methods
A qualitative study employed semi-structured interviews with 20 residents working in two tertiary university hospitals. Inductive analysis of interview records determined key themes, identified categories, and performed a type analysis.
1. Participants
From October to November 2017, in-depth interviews occurred with the residents from two university-based hospitals in Seoul, Korea. The study recruited participants actively engaged in clinical practice through purposeful sampling. Recruiting was done through posters, flyers, verbal presentations, and snowball sampling to prevent the possibility of coercion. Through iteration between pre-existing theories and the data, interview recruitment and data collection continued until no new concepts emerged so that the data were saturated. As a result, 20 participants were interviewed voluntarily through written consent. The study was reviewed and approved by the institutional review board at Korea University (1040548-KU-IRB-17-189-A-1).
Table 1 shows the characteristics of the participants, which include specialties: eight family medicine, two internal medicine, three obstetrics and gynecology, four orthopedics, two anesthesiology, and one ophthalmology. Three of the participants were first-year residents, four were second-year residents, nine were third-year residents, and four were fourth-year residents. Most participants were male (65%), with 35% female. Sampling served to achieve a mix of more-experienced and less-experienced residents and a mix of surgical and medical departments.
2. Data collection
K.M., a graduate and former trainee in the same hospital as the participants, interviewed the participants. To minimize the possibility of self-censorship due to the hierarchical nature of the interviewer-interviewee relationship, K.M. maintained an empathetic attitude and displayed respect throughout the interview, not disclosing his past status to the participants, using proper language, and assuring confidentiality. Consequently, all participants made concise and honest statements about their experiences, thoughts, feelings, and behaviors.
The interviews were semi-structured and conducted in a free dialogue format. After discovering relationships between several concepts during the research process (e.g., between uncertainty in medical practice and hierarchy, work satisfaction, and communication), additional questions provided deeper insight (Table 2). Open questions and the attempt to maintain a phenomenological attitude served to bracket researchers’ prejudices, respect participants’ experiences, and approach subjects’ perceptions in the context of their lives. Each interview session took 20 to 70 minutes until no more narratives on experiences of uncertainty emerged. Interviews were audio-recorded and transcribed by K.M., and all research materials were anonymized using codes and shared only with research team, including Y.M., who helped analyzing the data throughout the study.
3. Data analysis
K.M. organized the data into meaningful units in the initial coding after repeating thorough transcript reviews. Next, K.M. carefully performed line-by-line coding, labeling the concepts, and generating initial categories. Then, intermediate coding occurred using the qualitative research software, N-Vivo ver. 11.0 for windows (QSR International, Doncaster, Australia). After K.M. made an initial coding book, Y.M. and K.M. developed the category hierarchies, and inclusions of the themes emerged.
During the intermediate coding process, constant comparisons took place between the themes found in the interviews and previously published theories and then compared to the newly constructed themes. The discussion and analysis generated additional themes and categories. Iterative discussions between K.M. and Y.M. were conducted, and if any disagreement appeared, K.M. and Y.M. reviewed the original interview data, read it line by line, and discussed it until an agreement. Through axial coding, K.M. and Y.M. linked categories around an axis according to the properties and dimensions, uncovering conditions surrounding residents’ experiences of uncertainty and its response. Finally, K.M. and Y.M. performed a theoretical-type analysis of the participants’ coping behaviors according to the attributes revealed during the advanced coding process.
For member checking, eight participants received the intermediate coding results via e-mail for feedback on the analysis process. Feedback interviews with two participants involved explaining the study results after all analyses concluded, and they agreed with the findings.
Results
The participating residents’ experiences and responses to uncertainty in medical practice fell into major categories and corresponding sub-themes (Table 3).
1. Major categories and sub-themes
1) Experiencing uncertainties in medical practice
Residents reported various types of uncertainties in medical practice. Besides uncertainties in diagnosis, treatment, and prognosis, they reported uncertainties from communications, systems, ethical/legal, doctor-patient relationships, diversity of doctor’s personal experiences, mismatch of the data and reality, and medicine itself as a science. Among them, the diagnosis/treatment/prognosis-related uncertainties and system-related uncertainties were reported from most of the participants. A trainee stated about uncertainty arising from irrational resident training system.
“The truth is, first-year resident gets the surgery-consent, but he/she never gets to observe a surgery. So now, when he/she enters the operating room for the first time in his second year, he/she thinks, ‘Oh I have got my permissions all wrong…’” (#10)
2) Being faced with uncertainty
Residents reported various experiences facing medical uncertainty. Trainees were encountering medical uncertainties with perceiving their personal ignorance. One trainee stated as follows:
“When it seems there’s no problem, and can’t found the problem from the limits I see, it’s the scariest time. If the case is… the eyes appear shrunk in the CT scan, or the pus are full in the front (chamber) of the eye, I can say to the (patient) immediately. ‘I think we’ll have to go up to the operating room to get the irrigation done right away.’ But when I’m not sure why (the patient) can’t see, I get really scared when I notify.” (#9)
3) Context of medical environment
Participants were experiencing medical uncertainty in the context of the medical environment surrounding them. In the hospital, or in the context of the clinical environment surrounding oneself, the clinical practice was reported to be altered and constituted by it. The theme, ‘irrational medical care system’ was mentioned from six people, showing that physicians are strongly aware of the restrictive medical environment surrounding them. The story of one resident shows that this medical reality is eventually affecting the response to uncertainty.
“Patients should give more trust to the doctors and health insurance should be more supported from the society, but oppositely, you have to think about insurance first before you do the practice, and the atmosphere of society goes to the way that doctors are some bad people… and I think uncertainty could be derived from these.” (#6)
One of the residents talked about the harsh reality of junior residents in which it is impossible to accumulate knowledge or to study to solve medical uncertainties.
“I am busy with my work during the first year. You can’t open a book, you don’t even know why you’re doing this, and you are told, ‘This is the way that it is supposed to be.’ So, for the first or second year you go on like this…” (#8)
4) Coping with uncertainty
While struggling and grappling with uncertainty, most of the residents reported to cope with it, which could be considered constructive. Following reveals coping with uncertainty through ‘predicting growth as a doctor from experience’:
“Learn a lot, ask questions, experience… And finally, if we continue to experience this kind of uncertainty, won’t we learn? How to deal with it?” (#10)
Moreover, participants were accepting that medical uncertainty had to be acknowledged:
“But isn’t it possible that we are ignorant in some part? We have enormous things to study and in fact it doesn’t make sense that we know everything, and I think we should not think we could know everything. It’s science that keeps changing. There always will be possibility of ignorance. Of course, I will be always ignorant to (at least) something.” (#5)
On the other hand, at times residents reported somewhat unconstructive coping behavior when being faced with uncertainty. Following reveals coping with uncertainty through ‘abdicating the responsibility’:
“You know… when someone is hospitalized. Examining a patient in the emergency room doesn’t make him/her my patient.” (#10)
5) Self-reflection and self-directedness
Some of the participants saw themselves in terms of reflection and awareness of themselves in the face of uncertainty. Those who were satisfied with their work and self-directed to their callings showed rather constructive coping in the face of uncertainty:
“I’m happy not to leave work on time, to watch the patients late all the time, even if I am not on duty, to check-up the patient in the middle of the off time, to come and take care if the patient gets worse…” (#2)
Moreover, those who were willing to reflect on themselves and acknowledge their shortcomings were constantly growing faced with uncertainty:
“Currently, I do not have that standard… I am a doctor who has yet to establish his/her criteria.” (#8)
6) Communication and collaboration
Considering context of hospital environment which involves plentiful of people, including patients, colleagues (including other health-care providers), and/or superiors, communication and collaboration seem to have significant meanings in dealing with uncertainty facing in hospital life. Following case shows when the communications and cooperation within the medical team had helped solving uncertainty.
“I went out and thought to myself for half an hour and woke up both of my colleagues and asked them for help. It worked out, yeah. The absolute amount is (not the amount that could be handled by oneself). That’s… Just like you said, uncertainty… Since then, when I think I cannot handle it myself, I seek for help quickly.” (#7)
2. Revealing relations between categories
Axial coding elaborated the links and relations between categories by arranging themes and categories around the central phenomenon, ‘being faced with uncertainty’ (Fig. 1). In result, communication/collaborations, and communication/collaboration which depicted residents’ characteristics upon facing uncertainties in their medical practice, revealed to moderate subsequent coping behavior after being faced to uncertainty.
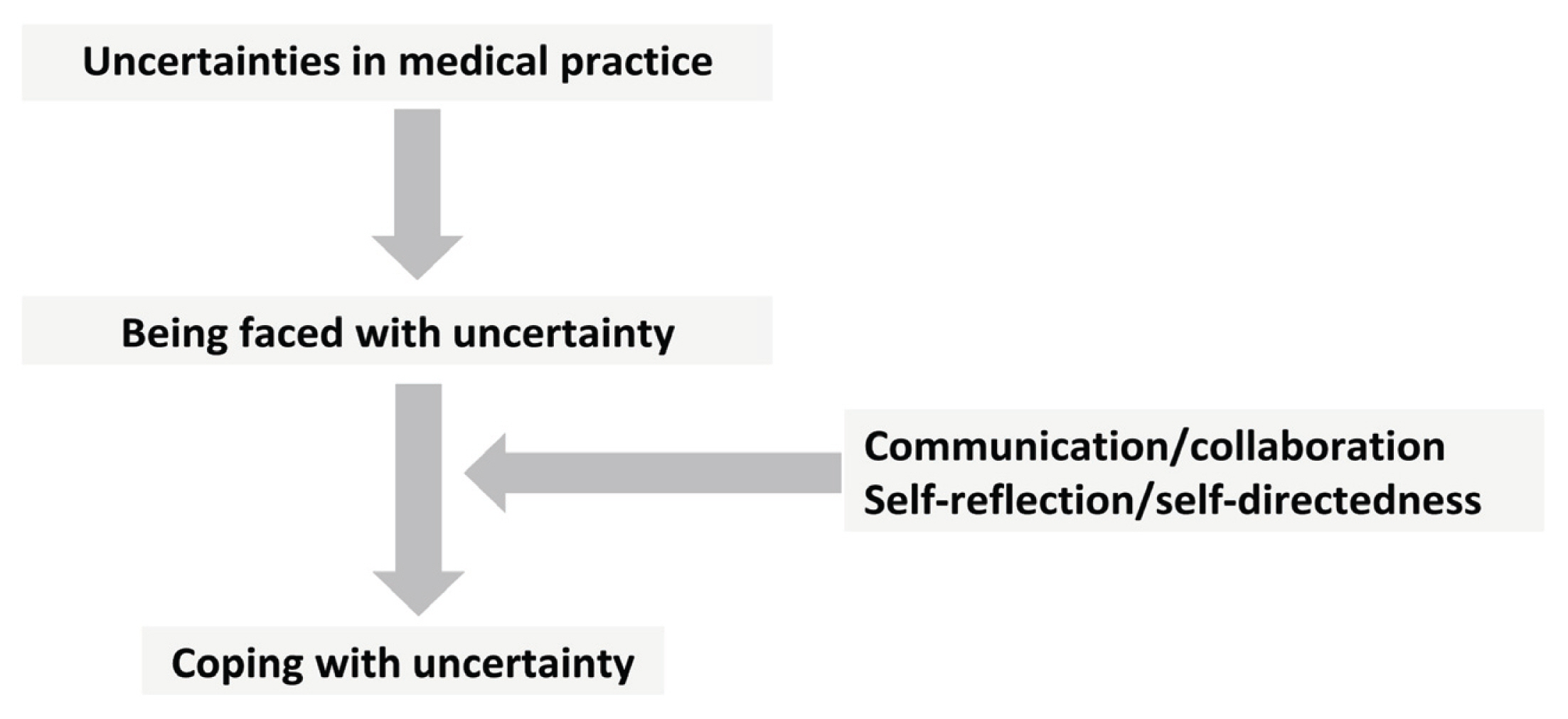
Relations between Categories
When the residents are faced with uncertainties in medical practice, immediate reaction occur which could be moderated by communicative/collaborative behaviors, and/or self-reflective/self-directed attitude, which can result in either constructive, or unconstructive coping with uncertainty.
3. Types of coping with medical uncertainty
According to the levels of self-reflection/self-directedness, and communication/collaboration, we classified four distinct uncertainty coping types of residents: adaptive, self-contained, submissive, and isolated (Table 4). Of the 20 participants who had enrolled in this study, we could categorize nine participants to four types explicitly. We couldn’t categorize rest of the participants discretely, due to the either lack of information or rather ambiguous coping behaviors.
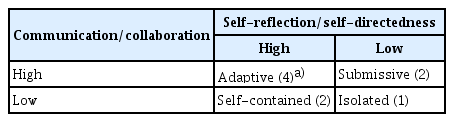
The Types of Uncertainty Coping Behaviors According to Participants’ High and/or Low Levels of Self-reflection/Self-directedness as Well as Their Levels of Communication/Collaboration
1) Adaptive type
We defined adaptive type as when both self-reflection/self-directedness and communication/collaboration behaviors are high. The residents in this category were well-aware of their strengths, weaknesses, and learning styles. They reflected on their experiences in practice. They showed good communication and collaboration with patients and colleagues. Moreover, they showed constant efforts to update knowledge in the face of uncertainty while acknowledging their limitations and uncertainties in health care and demonstrated flexible responses. Following instance shows a participant who thinks his/her strength lies upon his/her interest in patients also exhibits constructive coping with uncertainty by admitting innate nature of medical uncertainty.
“I work harder than anyone else, and I have a great deal of interest in the patients. Although I am not sure if I am better than others, I am always interested in my patients. I think that is my strength. I do not leave on time from work, and I always watch them until late. Even if I am not on duty, I come to the ward to watch over when the patient gets worse. I am so happy to do this.” (#2)
“If you are uncertain, follow up. At first, I thought it was my incompetence to observe and follow up, but I realized there are so many things that I cannot solve immediately.” (#2)
2) Submissive type
Some participants showed high levels of communication but somehow lacked self-reflection and self-directedness, tended to rely almost entirely on their seniors for medical decision-making.
“I believe I am dissatisfied because I am not good at it (my practice). I think that is why I always notify the professor immediately without my judgement.” (#19)
3) Self-contained type
Self-contained types were defined to have high levels of self-reflection/self-directedness but relatively low levels of communication/collaboration. Some participants of this type were either overly critical of the senior’s clinical decisions or were unable to establish a smooth relationship with others.
“Communicating with parents or patients is a mere psychological satisfaction. It is not a factor that helps me when I make a clinical decision.” (#16)
4) Isolated type
Isolated types were defined as when the participants exhibited both low levels of communication/collaboration and self-reflection/self-directedness. A small number of participants fell into this category as they failed to recognize their strengths and weaknesses, lacked pride in their work, and viewed it as unrewarding. Moreover, they expressed difficulty controlling their emotions, described low levels of achievement and poor communication with patients, and less effective collaboration with other healthcare professionals. During the interview, these participants expressed excessive shame about their medical practice when they relied on their superiors for most clinical decisions without independent judgment or responsibility.
“As a trainee, I felt I had no choice but to respect professors’ opinions. I thought it was a decision that was already out of my hands. So, I simply decided to follow the professor’s opinion. I would have told the professor about the situation if I had judged that, but I had not.” (#3)
Discussion
According to this study, when resident participants encounter various uncertainties in medical practice, their coping behavior could be attributed to their levels of self-reflective/self-directed attitudes and communicative/collaborative behaviors.
The participants who reflected on their training experiences to realize their specific capacities and limitations in medical practice and who had principles to act self-directed showed constructive coping behavior with uncertainty. It is known that self-directedness pairs with courage and diligence, which may promote professional development through tolerance of uncertainty [9]. Likewise, this study revealed that self-reflective and self-directed trainees demonstrated more constructive coping behavior to uncertainty, which may help them grow into more capable professionals.
Furthermore, communication and collaboration are vital to resolving uncertainty, especially in the acute and critical environments of the training hospital [17,18]. Recently, Kerr et al. [10] have shown that pediatric residents resolve medical uncertainties as their residency phases develop through time and gain uncertainty tolerance as they acquire communication efficacy with patients’ parents. Likewise, participants who could actively communicate and collaborate with patients, colleagues, supervisors, and other medical professionals demonstrated more constructive coping behaviors to uncertainty.
Based on their self-reflective/self-directed attitudes and communicative/collaborative behaviors, residents fell into four uncertainty coping types: adaptive, self-contained, submissive, and isolated. Adaptive participants with high self-reflection/self-directedness and high communication/collaboration showed more constructive behavior to uncertainty. In contrast, isolated type participant with low self-reflection/self-directedness and low communication/collaboration showed rather unconstructive coping behavior to it. Self-contained and submissive trainees showed mixed coping behavior to uncertainty.
Medical students and trainees commonly achieve professional growth by grappling with medical uncertainties [3,19]. As a result, adaptive type participants are likely to experience relatively good professional growth compared to self-contained type participants. Likewise, the submissive type participants may expand moderately, and the isolated type participants may grow insufficiently.
Several implications could be made. The submissive type should foster a more self-directed attitude through interventions such as keeping a portfolio of their practice and possible errors [20]. For self-contained type trainees, it will be beneficial to engage in more discussions and ask for help when they are uncertain or unclear. An isolated type of trainee should try to cultivate both communication/collaboration and self-directedness/reflections.
There are some limitations to this study. Despite the effort to maintain a phenomenological attitude, there may still be self-censorship among participants due to researchers’ affiliations and status. Regardless, all participants spoke clearly and frankly about their experiences, thoughts, feelings, and behaviors regarding uncertainties. Although recruitment of participants continued until the desired theoretical saturation occurred, a more comprehensive interpreting process (e.g., theoretical type analysis) revealed that participants’ coping behaviors including four types, may not have been sufficient to generate a complete substantive theory.
In conclusion, this study gives insights to cultivate constructive coping behavior when faced with uncertainty by fostering communicative/collaborative behaviors and self-reflective/self-directed attitudes.
Acknowledgements
I wish to thank Prof. Hyunmi-Park and Prof. Hyoung Seok Shin for thoughtful review of the transcript. In addition, I appreciate Prof. Hong Sik Lee, Prof. Yeon Sun Choi, and Prof. Kyung Wha Park, at the Korea University College of Medicine, for their contribution to elaborate the theory, based upon their residency teaching experience and through insights. And, I would like to express thanks to Prof. Su Jin Chae and Hee-young Han’s insightful comments on the qualitative analysis of the data. Finally, and most importantly, I would like to express my deepest appreciation to Prof. Young-Mee Lee for her contributions on overall process of the planning, designing, and analyzing in the most earlier process of the study.
Notes
Funding: No financial support was received for this study.
Conflicts of interest: No potential conflicts of interest relevant to this article was reported.
Author contributions: All work was done by Kangmoon Kim.



